A mother’s harrowing RSV story ends with a simple lesson
I began to wonder if this trip to a pediatric urgent care with my son was even necessary.
Sure, he had been diagnosed with pneumonia a week ago and didn’t seem to be getting better. His cough sounded uglier. But here Ethan was in classic 2 1/2-year-old mode: running in big circles around the waiting room chairs and causing the kind of ruckus only a toddler can.
He’d stuff some Pirate’s Booty I had hastily thrown into my purse in his mouth, before returning to his wild banshee ways and dashing around in circles again.
Our pediatrician said their office was too swamped with sick kids to see us, and referred us to this place. We had been told the wait to see a doctor would be a minimum of an hour. We struggled to find a seat in the packed waiting room as far as possible from other coughing kids.
We finally graduated from the waiting room to the doctor’s office, only for Ethan to continue his marathon by scooting a rolling chair back and forth, roaring with laughter every time it hit the examining table. When the physician walked in, I felt like I needed to defend wasting her time with this visit with my seemingly A-OK, albeit destructive, son.
But Ethan wasn’t OK.
The doctor listened to his chest with her stethoscope and didn’t like what she heard: wheezing, some crackling.
She showed me how Ethan’s Pirate’s Booty-stuffed stomach moved heavily each time he inhaled and exhaled.
They had Ethan complete a nebulizer treatment in the office, which meant slipping a device on his face that resembled an oxygen mask, while medicated air meant to open up his lungs flowed through a frightfully loud machine. I held him in my lap while the nebulizer was on, scrambling to find 100 different versions of “Wheels on the Bus” videos on YouTube to try to distract him from the vacuum-like whirring of the machine.
The doctor listened to his lungs again. His breathing still didn’t sound great, but she said the hospitals were too inundated right now.
I knew all too well what she meant. A few days before our urgent care visit, I had flagged a report for editors at The Hill that said children’s hospitals in the Washington area were at capacity, flooded with young kids suffering from RSV, a potentially life-threatening respiratory illness that has no vaccine.
After a three-hour visit, she gave Ethan a steroid and told us to follow up with his pediatrician the next day.
By the time we got to the pediatrician’s office the following morning, my happy-go-lucky, playful little guy was anything but. He curled up in my lap as we went through a similar routine that the urgent care doctor had done just the night before. His oxygen levels were too low, and our pediatrician had him do another nebulizer treatment.
“Our goal is to keep you from going to the hospital,” our pediatrician told us.
It seemed like an unusual “goal” from a doctor, but I understood her reasoning. But after Ethan’s oxygen levels dipped lower still after the nebulizer, she said we should rush him straight to the hospital after all.
My “Blue’s Clues” and vehicle-obsessed son, usually the epitome of toddler “I can do it myself!” independence, wouldn’t let me put him down for even a moment as we waited in the emergency room lobby. Surprisingly, a separate waiting area in the ER just for children wasn’t completely full, and I wondered if maybe news reports of endless waits were overblown.
Not so.
“He’s so cute,” a young mother in the waiting room told me, as she motioned to Ethan’s head of curls. She cradled her two-month-old in her arms, patiently rocking the baby after telling me she had waited three hours so far.
I held Ethan as my husband rushed from work to the hospital, meeting us there and with us as we were brought to an ER triage area. They ran more oxygen tests on Ethan, got some of his history, and then sent us back to the waiting room.
Finally, they called Ethan’s name and we were in the ER. My vibrant, otherwise-healthy kid was lethargic, laying on me with a glazed look in his eyes. We struggled to fit the two of us on an exam table meant for a single adult. They draped a lead apron over me and Ethan as they took X-rays of his tiny lungs. The nurse placed a cannula in Ethan’s nose for supplemental oxygen and put an IV in his arm to give him fluids, before wrapping it with a diaper so he wouldn’t try to take out the tube.

My husband and I, loopy from what was happening, laughed at the sight of a diaper being used MacGyver-style. “Hey, it works!” the nurse said, explaining that he’d done the maneuver with kid after kid in recent weeks.
The ER doctor finally came in our room and delivered a crash course in what might be to come. “Everywhere is full. The entire Eastern seaboard,” he said of hospitals.
“We’ve been airlifting kids to Pittsburgh, sometimes to Richmond,” he added. This hospital had a pediatric unit, but not an intensive care geared towards kids. So if Ethan’s condition became even more dire, they wouldn’t be able to treat him there. Our only hope was that the pediatric unit, which had just a few remaining beds, accepted him.
It was a gut punch. As the doctor left, my husband looked at Ethan, who had fallen asleep with a mask on as the nebulizer loudly buzzed away for another treatment.
“He’s just a baby. He’s not supposed to be here,” my husband said, defeated.
The pediatric unit doctor finally came into our room. She examined Ethan, and briefed us on how they’ve been dealing with case after case of the same thing: RSV.
But she offered us hope: He could head to the pediatric unit at the hospital. We wouldn’t need to travel for his care, as long as he didn’t worsen. Ten hours after we first entered the hospital, we had a bed for Ethan.
We’re among the lucky ones. We were told beyond airlifting, plenty of families had been spending multiple nights in the ER because there were no beds.
In Maryland, Gov. Larry Hogan (R) announced last week that hospitals would receive $25 million in additional funding from the state to prioritize pediatric intensive care unit staffing. Children from birth to age two comprised 57 percent of hospitalizations last week, according to Hogan’s office.
Next to the ghost decorations for Halloween adorning the doors of the pediatric unit, room after room had the same notice taped up: isolation guidelines. The rooms were all filled with kids facing the exact same thing as Ethan. RSV was everywhere.
There’s no cure for RSV. Every two hours on the dot, the nurses would give Ethan the nebulizer treatment.
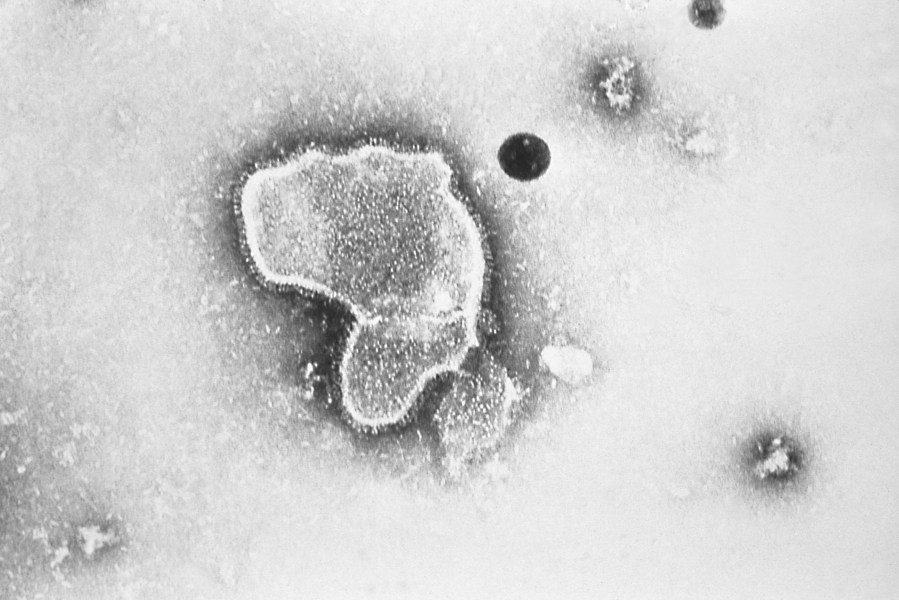
New research announced by Pfizer showed vaccinating pregnant women helped protect their newborns from the common but scary respiratory virus that fills hospitals with wheezing babies each fall. (CDC via AP)
A monitor affixed to his foot would alert nurses if his oxygen dipped dangerously low, which it did several times throughout the first night. I thought at one point to ask what happens if Ethan stopped responding to the treatments, but then didn’t ask because I didn’t want to know the answer.
The goal was to get him going without the need for additional oxygen, and breathing well for at least four hours between treatments, two times in a row.
That seemingly simple goal proved elusive for two full days. I originally thought it would be a nightmare trying to get a two-year-old to stay in a hospital bed for more than five minutes, but Ethan was in such bad shape that he barely made a fuss. Then, after midnight on our second night in the hospital, Ethan suddenly perked up.
He sat up and rolled over in the hospital bed. Then, he rolled onto my head, spreading his arms and legs out as far as he could stretch, and giggled.
“Should I sleep here?” he said, cracking himself up.
It was like someone hit the power button on my kid, and suddenly he snapped back to himself. I didn’t care that it was midnight and we needed to get some extremely interrupted sleep before the next nebulizer treatment. My son was back.
A nurse later told me that she enjoyed working with kids because for as quickly as their health can deteriorate, they can just as speedily bounce back.
After that, the doctor advised us to try stretching out his time between treatments. Finally, we were told he was stable enough to go home. I somehow hadn’t shed a tear the entire time we were at the hospital, but when the doctor signed off on us leaving, I bawled.
As nightmarish an experience as it was, I realize how incredibly fortunate my family is.
My husband and I have jobs that allowed us to drop everything when our son needed help. We have health insurance policies, and resources to get through spending days at the hospital.
Perhaps most importantly, we had access to an incredible team of doctors and nurses and the sheer fortune of being able to get a bed for our son during an unprecedented and unthinkable time for hospitals.
At the risk of repeating one of those parenting cliches that I would’ve rolled my eyes at a week ago, I’m thankful that I trusted my gut. Even when Ethan was being a wild child at urgent care, I knew something just wasn’t right. What I didn’t know was how much he had been struggling to breathe.
At the hospital after being discharged, Ethan and I waited in the lobby as my husband went to get our car from the parking lot to pick us up. Ethan spotted some empty wheelchairs in the corner of the lobby, and immediately ran over to them. He giggled as he tried to roll one of the chairs into the automatic opening and closing doors. As I looked on as he laughed and laughed at the pint-sized commotion he created, I breathed a sigh of relief.
Copyright 2023 Nexstar Media Inc. All rights reserved. This material may not be published, broadcast, rewritten, or redistributed. Regular the hill posts







